
Differences Between Panic Disorder and Generalized Anxiety Disorder
Among anxiety disorders, the contrasting threads of Panic Disorder and Generalized Anxiety Disorder

Migraines, characterized by throbbing headaches, sensitivity to light and sound, and sometimes accompanied by nausea, can be debilitating for those who suffer from them. The quest for effective migraine relief has led to various treatment approaches, one of which is Transcranial Magnetic Stimulation (TMS). TMS has garnered attention as a non-invasive and potentially groundbreaking method for managing migraines.
In this blog, we will discuss the benefits and potential side effects of TMS for migraines. Whether you’re seeking alternative treatments or merely curious about emerging migraine therapies, this blog is for you!
Transcranial Magnetic Stimulation (TMS) has emerged as a promising avenue in the pursuit of effective migraine treatment. This non-invasive procedure involves the use of magnetic fields to stimulate nerve cells in the brain, targeting specific areas believed to be associated with migraine pathology. Research studies and clinical trials have explored the efficacy of TMS in alleviating migraine symptoms, and the results are both intriguing and encouraging.
By modulating neuronal activity, TMS aims to disrupt the abnormal brain patterns often implicated in migraine episodes. As we delve into the question of whether Transcranial Magnetic Stimulation can truly treat migraines, we will examine the scientific evidence and delve into the mechanisms that underpin this innovative approach.
Understanding the therapeutic potential of TMS for migraines involves exploring how magnetic stimulation influences the brain’s neural circuits. The procedure typically involves placing a magnetic coil on the scalp, which generates magnetic pulses.
These pulses, when directed at specific brain regions, are thought to influence the excitability and activity of neurons. For migraine sufferers, whose condition is often linked to abnormal brain activity, TMS holds promise as a modulator of these irregular patterns. As we navigate through the research and insights surrounding TMS as a migraine treatment, we aim to provide a comprehensive understanding of its mechanisms and shed light on whether it stands as a viable solution for those seeking relief from the relentless grip of migraines.
The evidence supporting Transcranial Magnetic Stimulation (TMS) for chronic migraines is promising but nuanced. Positive outcomes from randomized controlled trials reveal a potential reduction in frequency and severity of migraines, with a meta-analysis indicating an average decrease of 8 migraine days per month. Some studies show improvements in disability and quality of life.
However, mixed findings and varying effectiveness based on stimulation parameters suggest a need for refinement. Limitations include the relatively small size of studies, necessitating larger investigations for conclusive results.
Despite its potential, more research is essential to determine optimal protocols and assess long-term safety and efficacy, as the exact mechanism of TMS in migraines remains unclear.
Transcranial Magnetic Stimulation (TMS) operates on the principle of utilizing magnetic fields to influence neural activity in the brain. This non-invasive procedure involves the use of a magnetic coil placed against the scalp, through which short electromagnetic pulses are delivered to specific brain regions.
The magnetic pulses induce electrical currents in the neurons, modulating their activity. In the context of migraines, TMS is thought to disrupt the abnormal patterns of neuronal firing associated with migraine episodes. By targeting areas implicated in migraine pathology, such as the prefrontal cortex, TMS aims to restore a more balanced and normal state of neural activity, potentially providing relief for individuals experiencing migraines.
The intricacies of how Transcranial Magnetic Stimulation works underscore its potential as a therapeutic intervention, offering a novel approach to migraine management.
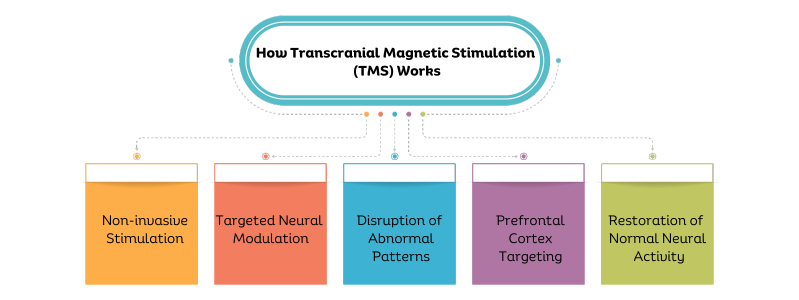
Non-invasive Stimulation: TMS involves the application of magnetic pulses to the scalp, requiring no surgical procedures.
Targeted Neural Modulation: The magnetic pulses induce electrical currents in specific brain regions, influencing the activity of neurons associated with migraines.
Disruption of Abnormal Patterns: TMS aims to disrupt the irregular firing patterns of neurons believed to contribute to migraine episodes.
Prefrontal Cortex Targeting: Specific areas of the brain, such as the prefrontal cortex, are often targeted in TMS for migraines to address underlying neurological factors.
Restoration of Normal Neural Activity: By modulating neuronal activity, TMS seeks to restore a more balanced and typical state of brain function, potentially alleviating migraine symptoms.
The journey of Transcranial Magnetic Stimulation (TMS) for migraine management necessitates a mindful consideration of essential precautions. Ensuring safety and optimizing the potential benefits of TMS involves a comprehensive approach, beginning with a thorough medical consultation.
Medical Consultation:
Prior to undergoing Transcranial Magnetic Stimulation (TMS) for migraines, it is essential to consult with a qualified healthcare professional. They can assess your medical history, current health status, and any pre-existing conditions to determine if TMS is a suitable option for you.
Detailed Health Assessment:
A comprehensive health assessment should be conducted to rule out any contraindications or potential risks associated with TMS. This evaluation may include neurological examinations, medication reviews, and an analysis of any implanted devices.
Pregnancy Considerations:
For individuals who are pregnant or planning to become pregnant, discussing the potential risks and benefits of TMS with a healthcare provider is crucial. The impact of magnetic stimulation on pregnancy should be thoroughly evaluated.
History of Seizures:
Individuals with a history of seizures may need careful consideration before undergoing TMS. Seizure risk is a critical factor, and the healthcare provider will assess whether TMS is a safe option in such cases.
Evaluation of Medications:
Certain medications may interact with TMS or affect its efficacy. A thorough review of the medications you are currently taking should be conducted to ensure compatibility with TMS treatment.
Psychiatric Evaluation:
As TMS is sometimes used in the treatment of psychiatric conditions, a mental health evaluation may be necessary to assess the potential benefits and risks, especially if you have a history of psychiatric disorders.
Informed Consent:
Before proceeding with TMS, it is crucial to fully understand the procedure, its potential outcomes, and any associated risks. Informed consent is a fundamental step in the decision-making process, ensuring that individuals are aware of what to expect from TMS treatment for migraines.
Monitoring During Treatment:
Continuous monitoring by trained healthcare professionals during TMS sessions is standard practice. This ensures immediate response to any unexpected reactions and contributes to the overall safety of the procedure.
Post-Treatment Observation:
Following TMS sessions, individuals may be observed for a period to monitor for any immediate side effects or complications. This post-treatment observation adds an extra layer of precaution to the TMS process.
While Transcranial Magnetic Stimulation (TMS) offers a non-invasive and promising avenue for migraine relief, it is vital to address the potential side effects and risks associated with the procedure. Understanding these factors is crucial for individuals considering TMS as part of their migraine management strategy.
Although TMS is generally considered safe, like any medical intervention, it may have side effects and risks that need to be carefully evaluated.
Headache and Scalp Discomfort: Mild headache and discomfort at the treatment site are common side effects, typically short-lived and diminishing after the session.
Muscle Twitching or Jaw Contractions: During TMS, some individuals may experience muscle twitching or contractions, particularly around the face or jaw. These effects are generally temporary.
Lightheadedness or Dizziness: A sensation of lightheadedness or dizziness may occur during or after TMS sessions, and it usually resolves quickly.
Potential for Seizures: While rare, there is a small risk of TMS triggering seizures, particularly in individuals with a history of epilepsy or a predisposition to seizures.
Hearing Changes: TMS may produce clicking sounds during the procedure, which can cause temporary changes in hearing. These changes are generally mild and transient.
Scalp Discomfort or Tingling: Some individuals may experience discomfort or tingling sensations on the scalp during TMS, which typically subside after the session.
Influence on Cognitive Function: TMS may have subtle effects on cognitive function, such as changes in memory or concentration. However, these effects are generally temporary and resolve after the treatment course.
Adverse Reactions to Coil Placement: Improper placement of the magnetic coil or individual sensitivity may lead to adverse reactions. Ensuring proper positioning is crucial to minimize such risks.
Rare but Serious Complications: While rare, serious complications such as seizures or mania have been reported. Individuals with a history of psychiatric conditions should be closely monitored.
The consideration of Transcranial Magnetic Stimulation (TMS) for migraine management is a nuanced decision that involves various factors. Individuals who may find TMS a viable option are often those who have experienced limited success with traditional migraine treatments or those seeking alternative therapies.
TMS is typically considered for individuals with chronic migraines or those whose condition significantly impacts their quality of life. Moreover, individuals who prefer non-invasive treatments and are willing to explore innovative approaches may find TMS an appealing option.
However, it is crucial to consult with a healthcare professional to determine suitability, considering factors such as medical history, current health status, and the presence of any contraindications. The decision to pursue TMS for migraines should be a well-informed one, guided by an individualized assessment of the patient’s unique circumstances and medical considerations.
The exploration of Transcranial Magnetic Stimulation (TMS) for migraines reveals a multifaceted approach to managing this often-debilitating condition. The decision to embark on TMS as part of a migraine management strategy should be made in consultation with healthcare professionals who can assess its appropriateness based on the individual’s medical history and current health status. As TMS for migraines continues to be studied and refined, it stands as a testament to the evolving landscape of medical innovation, offering hope to those in search of effective and alternative solutions for managing the impact of migraines on their lives.

Among anxiety disorders, the contrasting threads of Panic Disorder and Generalized Anxiety Disorder

How To Be Productive When Depressed: Tips & Coping Strategies In productivity, finding the motivation to tackle even the smallest tasks can be challenging, and

Men’s Mental Health Matters: Breaking the Silence and Building Resilience In health and well-being, the spotlight has historically focused predominantly on physical fitness, leaving the
