
TMS for Migraines: Uses Benefits and Side Effects
TMS for Migraines: Uses Benefits and Side Effects Migraines, characterized by throbbing headaches, sensitivity to light and sound, and sometimes accompanied by nausea, can be
In mental health, the terms “delusion” and “hallucination” often create confusion due to their interchangeability. It’s essential to differentiate between these phenomena accurately. Delusion and hallucination represent distinct experiences within psychology and psychiatry.
Recognizing the subtle disparities between them is essential for accurate diagnosis and tailored treatment of psychiatric disorders. By discerning these differences, healthcare professionals can offer targeted interventions, fostering trust and collaboration with patients.
Ultimately, understanding delusion and hallucination is not just about academic knowledge but about providing effective support and promoting healing in the realm of mental health.
In the context of mental health, delusion is defined as a fixed belief or conviction that endures in the face of overwhelming evidence to the contrary. These beliefs often deviate from cultural norms and are not shared by others in the individual’s community or cultural group. Delusions can manifest in various forms, including paranoid delusions, grandiose delusions, and somatic delusions.
Understanding delusions is essential in psychiatric assessment, as they are hallmark symptoms of psychotic disorders such as schizophrenia and bipolar disorder. Identifying and addressing delusions early on can guide appropriate treatment interventions and support strategies for individuals experiencing these distressing symptoms.
Recognizing the signs and symptoms of delusion is crucial for accurate diagnosis and intervention. Individuals experiencing delusions may exhibit behaviors such as withdrawal, agitation, or preoccupation.
The origins of delusions are multifaceted, often stemming from complex interactions between genetic, biological, and environmental factors. Several key contributors include:
Addressing delusions involves a multifaceted approach aimed at challenging and modifying irrational beliefs while providing appropriate support and treatment. Cognitive-behavioral therapy (CBT) stands as a cornerstone in delusion management, focusing on identifying and altering maladaptive thought patterns.
Encouraging reality testing, where individuals critically evaluate the evidence supporting their beliefs, can help challenge delusions. Additionally, medication, such as antipsychotics, may be prescribed by a psychiatrist to alleviate symptoms associated with delusional thinking.
Psychoeducation, support groups, and holistic interventions further complement the treatment regimen, fostering empowerment and resilience in individuals navigating the complexities of delusional thinking.
Hallucination is a phenomenon prevalent in various psychiatric conditions that refers to the perception of sensory experiences that are not rooted in external reality. Unlike delusions, which involve fixed false beliefs, hallucinations involve sensory perceptions that occur without corresponding stimuli from the environment.
These sensory perceptions can manifest in different modalities, including auditory, visual, tactile, olfactory, and gustatory hallucinations. Hallucinations often carry a vivid and compelling quality, leading individuals to experience them as real despite their lack of objective existence.
Understanding hallucinations is pivotal in psychiatric assessment, as they are characteristic symptoms of conditions such as schizophrenia, substance-induced psychotic disorders, and certain types of mood disorders.
Differentiating hallucinations from other perceptual disturbances is essential for accurate diagnosis and tailored treatment interventions in mental health care.
Hallucinations encompass a spectrum of perceptual disturbances that can significantly impact an individual’s perception of reality.
The causes of hallucinations are diverse and often interconnected, reflecting the complex nature of the human mind and its susceptibility to various influences. Key factors contributing to the occurrence of hallucinations include:
Addressing hallucinations necessitates a comprehensive approach tailored to the individual’s specific circumstances and underlying causes. Treatment strategies typically involve a combination of pharmacological interventions, psychotherapy, and psychosocial support.
Antipsychotic medications, prescribed by a psychiatrist, are often utilized to alleviate hallucinatory symptoms by modulating neurotransmitter activity in the brain. Additionally, psychotherapy, particularly cognitive-behavioral therapy (CBT), can help individuals challenge distorted perceptions, develop coping strategies, and enhance reality-testing skills.
Psychosocial support, including education, family therapy, and support groups, plays a vital role in fostering understanding, acceptance, and resilience in individuals coping with hallucinations. Holistic approaches, such as mindfulness techniques, stress management, and lifestyle modifications, may also complement conventional treatment methods, promoting overall well-being and symptom management.
Collaborative efforts between healthcare providers, individuals, and their support networks are essential in navigating the complexities of hallucinations and facilitating long-term recovery and stability.
Delusions and hallucinations are distinct phenomena within the realm of mental health, each with unique characteristics and implications. Delusions involve fixed false beliefs that persist despite evidence to the contrary, while hallucinations encompass sensory perceptions without corresponding external stimuli.
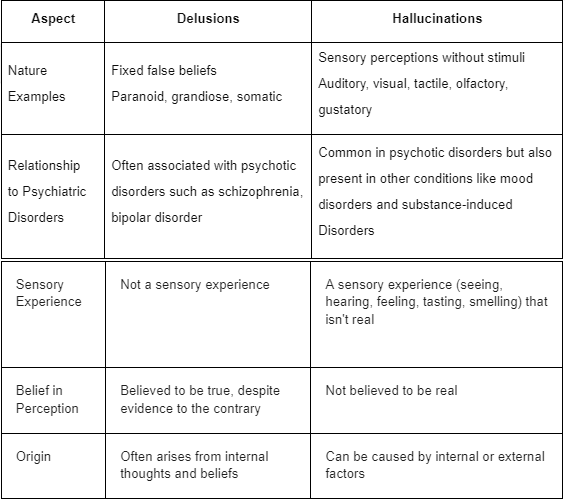
Hallucinations and delusions represent distinct manifestations of psychosis, each with its own array of subtypes and variations. Hallucinations involve perceptual distortions wherein individuals experience sensory perceptions without external stimuli, while delusions entail fixed false beliefs that persist despite evidence to the contrary.
Understanding the nuances of these phenomena is essential for accurate diagnosis and effective treatment in psychiatric practice.
Types of Hallucinations:
Types of Delusions:
Hallucinations and delusions are intimately linked to schizophrenia, a complex and debilitating psychiatric disorder characterized by profound disruptions in thought processes, perception, and behavior. In the context of schizophrenia, hallucinations often manifest as auditory experiences, such as hearing voices commenting on or commanding the individual’s actions.
These hallucinations can be distressing, compelling, and disruptive, contributing to the individual’s subjective experience of psychosis. Delusions, on the other hand, commonly occur alongside hallucinations in schizophrenia, further exacerbating the individual’s impaired perception of reality.
Paranoid delusions, for instance, frequently accompany auditory hallucinations in schizophrenia, fueling beliefs of persecution, conspiracy, or malevolent intent directed toward the individual. The co-occurrence of hallucinations and delusions in schizophrenia underscores the intricate interplay between neurobiological, genetic, and environmental factors contributing to the disorder’s onset and progression.
Understanding the relationship between hallucinations, delusions, and schizophrenia is pivotal in informing diagnostic assessment, treatment planning, and support strategies aimed at promoting recovery and stability in individuals grappling with this chronic mental illness.
Delusions and hallucinations represent intricate facets of the human mind, each with its unique characteristics, causes, and implications for mental health. Distinguishing between these phenomena is essential for accurate diagnosis, tailored treatment interventions, and compassionate support in psychiatric practice.
Whether manifested in conditions like schizophrenia, bipolar disorder, or psychotic depression, understanding the complexities of delusions and hallucinations is paramount in fostering empathy, awareness, and effective care for individuals navigating the challenges of mental illness.

TMS for Migraines: Uses Benefits and Side Effects Migraines, characterized by throbbing headaches, sensitivity to light and sound, and sometimes accompanied by nausea, can be

Why Do I Hear Voices in My Head? Get Instant Relief Now! Have you ever experienced the sensation of hearing voices in your head? You

What is Bipolar Anger? Reasons Behind Bipolar Rage Get Instant Relief Now! Bipolar rage is a distinctive manifestation of bipolar disorder which is a mental
