Managing derealization especially when triggered by factors like depersonalization from weed, requires a multifaceted approach that addresses both the underlying causes and the immediate symptoms.
Cognitive-behavioral therapy (CBT): CBT helps individuals identify and challenge distorted thoughts and beliefs contributing to derealization. It also teaches coping skills to manage anxiety and stress triggers effectively.
Antidepressants: Selective serotonin reuptake inhibitors (SSRIs) or serotonin-norepinephrine reuptake inhibitors (SNRIs) may be prescribed to alleviate symptoms of anxiety and depression, which often co-occur with derealization.
Anti-anxiety medications: Benzodiazepines or buspirone may provide short-term relief from anxiety symptoms associated with derealization.
Mindfulness meditation: Practicing mindfulness techniques can help individuals ground themselves in the present moment, reducing feelings of detachment and promoting a sense of connection to reality.
Progressive muscle relaxation: This technique involves tensing and relaxing different muscle groups to alleviate physical tension and promote relaxation, which can help counteract the dissociative symptoms of derealization.
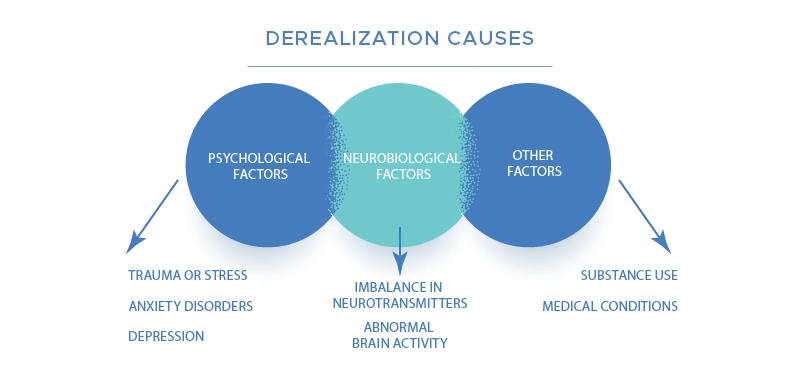
Avoiding substance use: Avoiding substances known to exacerbate derealization, such as cannabis and hallucinogens, can help prevent further episodes of depersonalization triggered by substance-induced dissociation.
Establishing a healthy routine: Prioritizing regular sleep, nutritious diet, exercise, and stress management techniques can support overall mental health and reduce the likelihood of experiencing derealization episodes.
Support Groups: Joining support groups or online communities for individuals experiencing derealization can provide validation, understanding, and practical coping strategies from others who have shared similar experiences.
Self-Care Practices: Engaging in activities that promote relaxation and self-care, such as spending time in nature, practicing creative expression, or engaging in hobbies, can help individuals reconnect with themselves and their surroundings, reducing feelings of detachment and unreality.